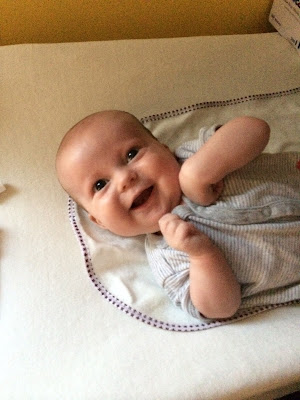
Yesterday reminded me of the earliest days of this little adventure, when I was still reeling and taken aback every time there was yet another complication or side-effect to Sam's condition.
Sam is still on oxygen--has been for about a week. He's on the lowest possible amount, and only needs it sometimes, but he hasn't been able to kick the habit even though the assumed cause of the problem, his head cold, seems to be fading. Docs have not perceived anything with the stethoscope or chest x-rays, so they gave him a CT scan.
They saw nothing of concern in Sam's lungs, but they did see something wholly unexpected: a compression fracture of one vertebra (T-8). Given his size (12 lbs.) and understandably sedentary lifestyle, the only plausible explanation we've been given is that Sam's bones have been weakened from the steroids he's been getting on and off for three-plus months, when they were used in "massive quantities" (our doc's words) to fight off the HLH and keep it suppressed before the transplant.
Sam is not evidently in pain, and there's not much to do about the fracture*--we don't need to put him in a brace, subject him to surgery, restrict his movement, hold him only in certain ways, etc. The docs don't seem alarmed by the fracture, but they are going to start increasing his Vitamin D and calcium intake and try--or at least hope--to minimize Sam's exposure to steroids.
Even so, we still have no idea how it happened or if it's going to happen again. And, if it does, how or if we'll know it. It may be true that weak bones are an expected side effect to prolonged exposure to steroids, but that is only minimally reassuring, if at all. And no matter what we
hope to do, it's unlikely that we'll be able to forego steroids, which are a big part of the post-transplant regimen. So Sam will continue to be fragile (but how fragile?) for the foreseeable future.
Fortunately, the news is not all bad. The mucositis does not seem to have gotten worse, and we're not seeing any of the other chemo side-effects. It's obvious that Sam doesn't feel well, but he sleeps a lot and doesn't have to suffer through it much.
Even better: today's lab tests showed early indications that his body is gearing up to produce blood again--i.e., that the transplant is taking hold. This is exciting news, but it also comes with a price: if engraftment occurs
too quickly, Sam may experience "engraftment syndrome," whose symptoms (fever, rash, fluid retention) aren't serious, but which would be treated with medications that come with their own risks: diuretics, which are starting to take a toll on Sam's kidneys; and, yes, steroids.
In short, we are now treating the treatment and fighting the side-effects as much as the original diagnosis. Or, as my mom put it, "walking a tight rope."
* I had a compression fracture of two vertebrae when I was 20--skiing accident. I was taken to the hospital, given a shot of Demerol (which I highly recommend), and sent home the same day, presumably with a prescription for something less awesome than Demerol. That was it. There was (very) slight lingering pain and stiffness for a few years, but nothing more.